Client Background
The client is a mid-sized practice based in Virginia, specializing in primary care and chronic disease management. The practice is serving more than 3000 patients annually, delivering comprehensive, patient-centered care.
The client has earned significant popularity in the South Atlantic region for their commitment, willingness, and dedication towards obtaining the expected patient health outcomes by timely follow-up of patients.
Business challenges
With an increasing patient population, the client was struggling with documentation overhead, reducing the clinician’s productivity. Along with documentation, the client has faced several challenges:
1. High Costs for Transcription Services
To manage the high inflow of patients, the practice has relied on external transcription services that incurred monthly expenses. Each provider’s notes were manually transcribed after patient visits, adding layers of costs to their operating budget and limiting funds available for other initiatives.
2. Opportunity Cost of Provider Time
The practice was losing significant revenue as the clinicians spent their average 2 hours per day on manual documentation, which could otherwise be spent on patient consultations. This consumption of time on documentation restricted them from attending to more patients, which ultimately reduced revenue potential.
3. Delayed Data Entry
Manual documentation by clinicians leads to delays in updating patient records, thus creating a lag between patient visits and data availability. These delays impact billing accuracy, create difficulty in submitting claims promptly, and increase the risks of claims denials due to missing or incomplete documentation.
Solution
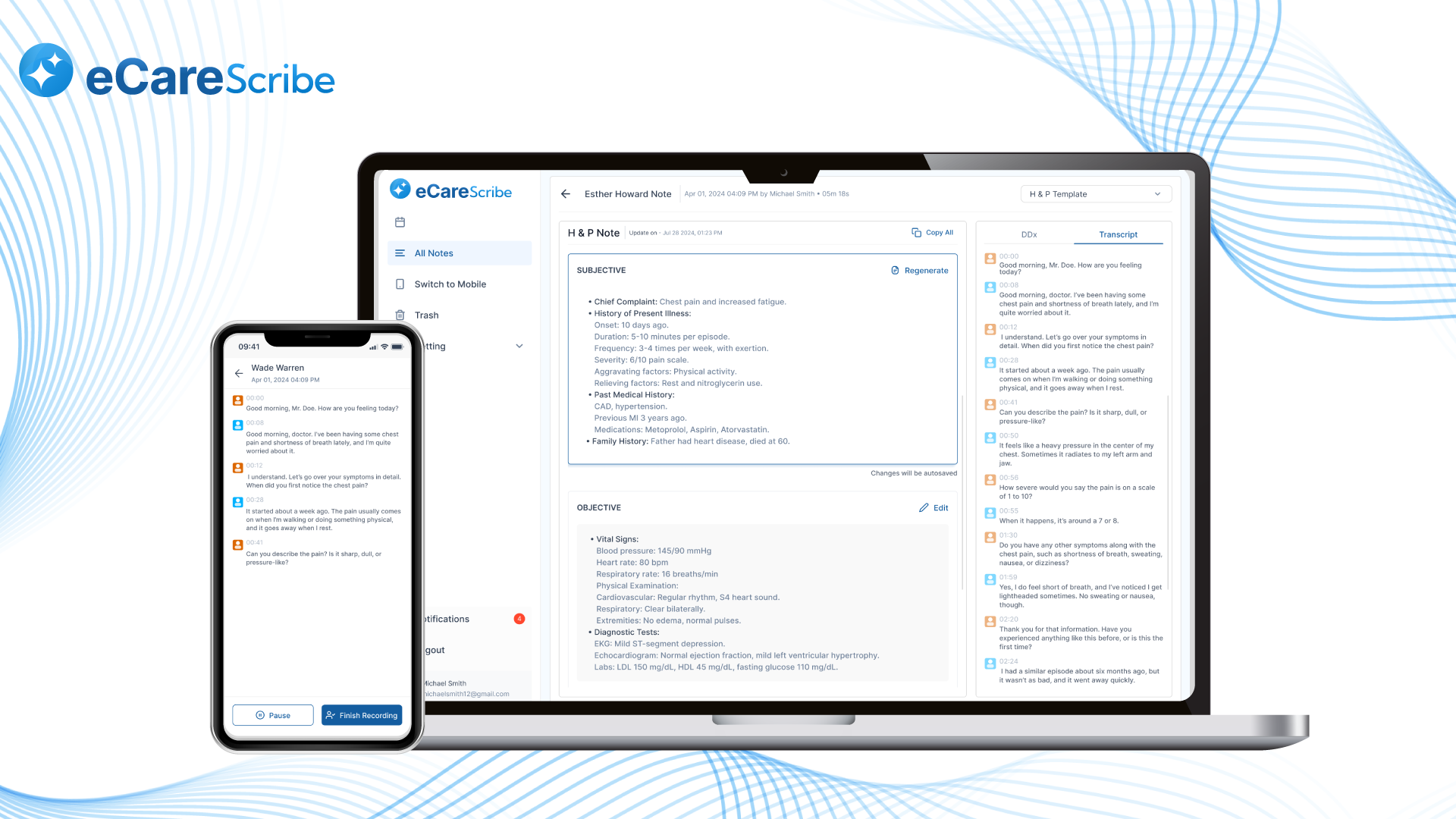
The client was looking for software that could automate the note-taking process and reduce their reliance on transcription services. The client has approached Medarch Inc. for an eCareScribe AI notetaker. Which leverages cutting-edge AI technologies and streamlines the documentation process for practice.
Solution Highlights
1. Automated and Real-Time Documentation
eCareScribe software helped clinicians to document patient visits in real-time using voice recognition and transcription features. During the patient visits, the eCareScribe captures key details like diagnoses, prescribed treatments, and follow-up actions. It not only generates notes but also organizes them in the customizable format of the clinician’s choice. This functionality has eliminated the need for external transcription services, ultimately reducing the costs associated with it.
2. EHR Integration for Immediate Data Updates
Not only documenting the medical notes of patients but also updating them to the patient records in EHR is also important. The eCareScribe, seamlessly integrated with the client’s existing Electronic Health Record (EHR) system, allows clinicians to update the patient records immediately post-visit. This immediate update of patient medical records ensured that clinicians were always accessible to deliver enhanced care and submit claims whenever required, reducing claim denials due to delays in documentation.
3. Enhanced Billing Accuracy with Structured Templates
eCareScribe provided customizable templates aligned with billing and coding requirements, ensuring that each patient’s details were captured accurately and comprehensively. This feature helped reduce coding errors, leading to more accurate billing, fewer denied claims, and maximized reimbursements.
4. Cost Savings and Improved Operational Efficiency
The elimination of transcription services generated immediate cost savings, while the improved documentation accuracy and efficiency streamlined practice operations. The AI notetaker contributed to a sustainable reduction in administrative overhead, allowing the practice to allocate resources to expanding patient services rather than covering documentation expenses.
Value Delivered
Through the implementation of eCareScribe AI notetaker, the client realized several measurable improvements:
1. Reduced Documentation Costs by 50%
By eliminating the need for transcription services, the practice saved thousands in monthly costs.
2. 40% reduction in documentation time
The automated note taking by eCareScribe has eliminated the manual note taking activity of clinicians,reduced time spent on documentation. It helped clinicians to interact more with patients and deliver patient centered care.
3. 25% Increase in Billing Efficiency
Immediate data entry into the EHR streamlined the billing process, reduced claim denial rates, and improved cash flow by expediting reimbursements.
4. Enhanced Data Consistency and Accessibility
Real-time updates and standardized documentation templates improved the quality and consistency of patient records, supporting better-informed clinical decisions and continuity of care.



