Client Background
The client is a mid-sized healthcare practice in Alaska that offers primary care and specialized services to a large patient population with chronic care needs. The practice operates in a fast-paced environment, requiring efficient documentation processes to manage patient data effectively while reducing administrative workloads for healthcare providers.
Business challenges
The client faced challenges in maintaining consistent and accurate documentation during patient consultations, especially given the increasing volume of patients. Key challenges included:
1. Time-consuming Documentation
Clinicians attended a high volume of encounters daily. During the encounters, manual note-taking consumed a significant amount of time for clinicians and restricted them from engaging with more patients and delivering comprehensive care.
2. Data Quality Concerns
Manual documentation leads to inaccuracies and errors. Inaccurate medical documentation created difficulties in audits and making informed decisions about the patient's health.
3. Provider Burnout
With additional administrative responsibilities, providers experienced increased levels of burnout, affecting their productivity and focus on patient care.
Solution
To overcome these challenges, the client approached Medarch Inc. for an eCareScribe AI notetaker, which uses advanced AI cutting-edge tools to improve medical documentation and reduce errors.
Solution Highlights
The client implemented an eCareScribe AI Notetaker software designed specifically for healthcare practices. Key features of the solution included:
1. Automated Documentation
eCareScribe captures every spoken word and transcribes it in text in real-time, making a detailed summary of the patient-provider conversation. It also highlights the key information, extracts action items, reduces the clinician's efforts, and allows them to engage more with the patient in encounters rather than doing administrative work.
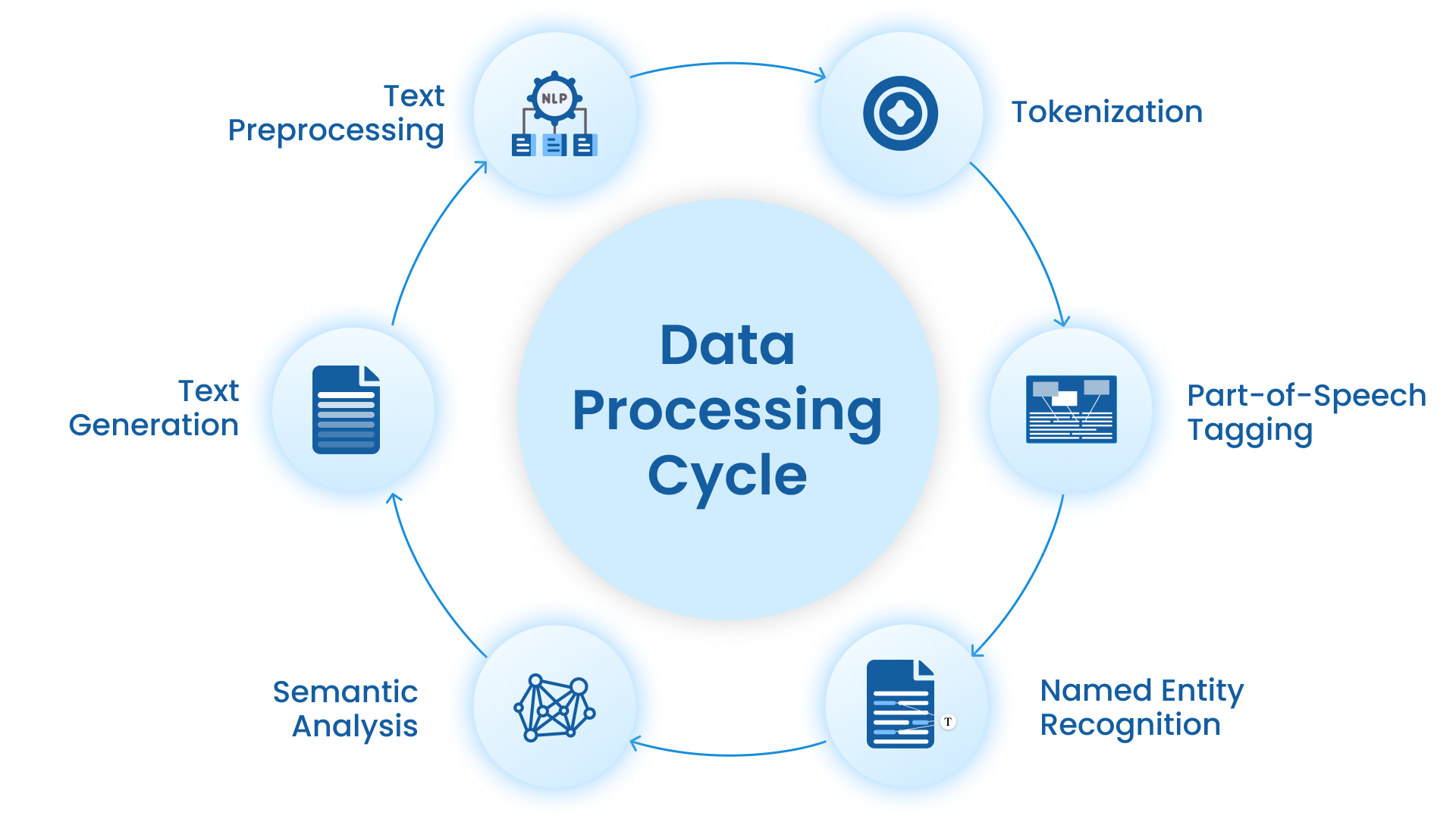
2. Natural Language Processing (NLP)
Using NLP, the AI Notetaker identifies and categorizes relevant clinical information (e.g., diagnoses, symptoms, treatment plans) to ensure complete, standardized records.
3. EHR Integration
The AI Notetaker seamlessly integrates with the practice's EHR, allowing for automatic syncing of notes and ensuring compliance with healthcare regulations.
Value Delivered
1. Improved Efficiency
The eCarescribe AI Notetaker reduced the documentation time per patient by over 40%, allowing providers to see more patients or allocate more time to each consultation.
2. Enhanced Data Accuracy
Automated and standardized notes led to a 30% improvement in data accuracy, reducing the potential for errors and improving care quality.
3. Provider Satisfaction and Reduced Burnout
With less time spent on administrative tasks, providers reported a 25% improvement in job satisfaction, focusing more on patient care and less on documentation.
4. Increased Revenue Opportunities
By capturing all relevant documentation accurately, the practice saw improved claim acceptance rates, resulting in a 15% increase in reimbursement rates.



