Client Background
A mid-sized multi-specialty healthcare practice in Virginia, U.S., has been experiencing high rates of provider burnout, particularly for those involved in patient care. The practice is known for its comprehensive care services. Still, its administrative workload grew exponentially as it handled complex chronic cases, leading to increased documentation requirements and a strain on provider well-being.
Business challenges
While handling the high patient volume, the client identified several challenges that required
implementing AI notetaker software in their practice.
The primary challenge was provider burnout resulting from extensive manual documentation
processes. Each provider was required to complete detailed patient notes, spending 1-2 hours on
documentation daily outside patient hours. This extended work burden affected job satisfaction,
decreasing productivity and increasing staff turnover. Key issues included:
1. Excessive Documentation Time
During the encounters, the healthcare professionals were used to taking manual notes. Post encounters completing the documentation consumes a significant amount of time, restricting them from interacting more with patients. This excessive documentation time has affected patient care and satisfaction levels.
2. Data Inaccuracy
The manual documentation processes by healthcare professionals led to inconsistent entries, impacting care quality and increasing compliance risks.
3. Patient dissatisfaction
Provider burnout due to administrative overload was causing lower engagement with patients and high turnover, impacting the continuity of care. It ultimately affects the patient satisfaction levels and health outcomes.
Solution
To overcome these challenges and improve provider and practice efficiency by reducing administrative activities, the client has approached Medarch Inc. for eCarescribe software. Our team of business analysts showed the client a demonstration of the software. After the demonstration, the client gave approval to implement the software in their practice.
Solution Highlights
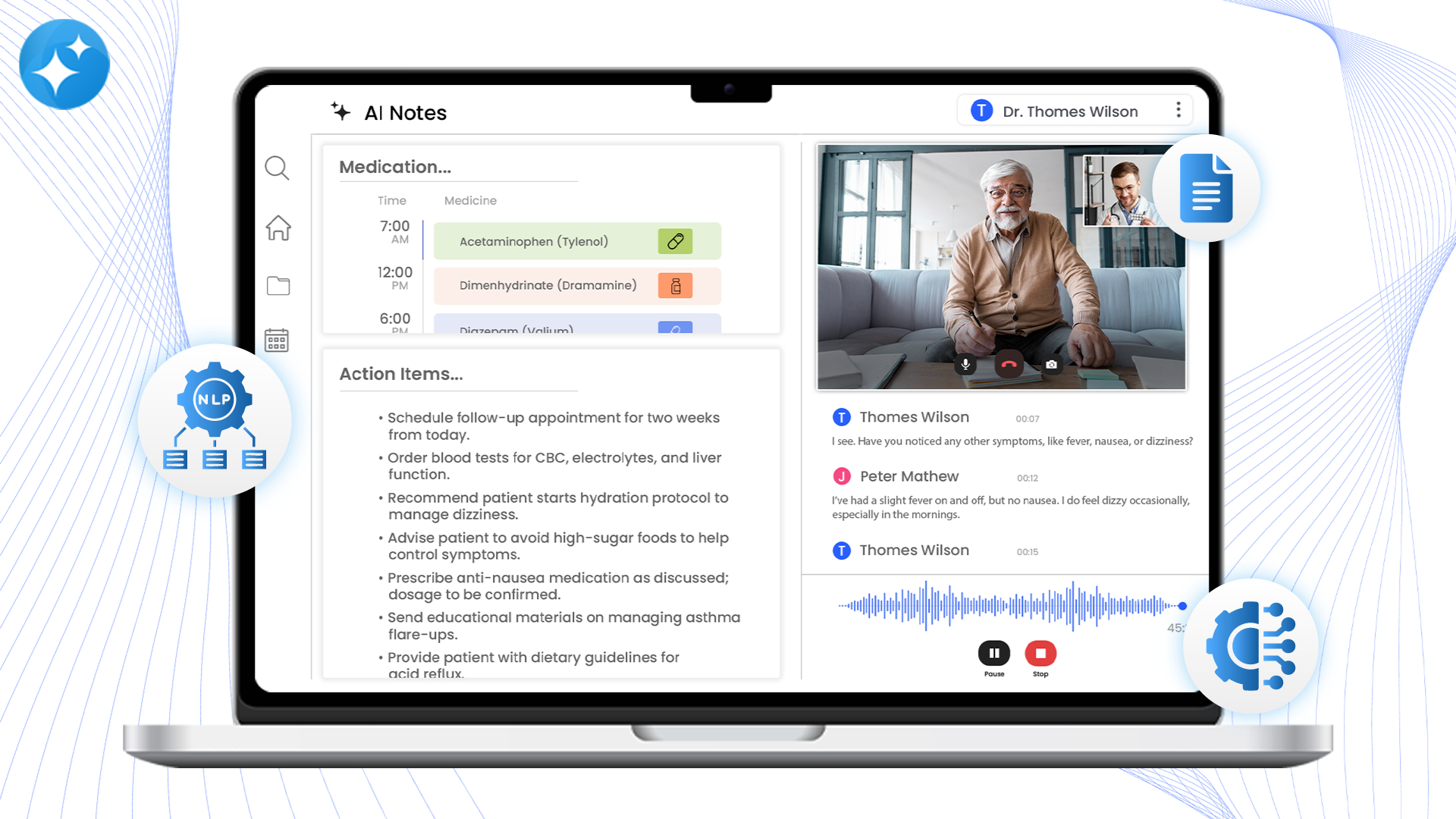
The practice implemented the eCarescribe AI Notetaker, an AI-powered documentation solution to streamline patient note-taking. Some of its key features included:
1. Automated Real-Time Documentation
The eCareSribe AI notetaker records and transcribes every spoken word in the text during the conversation, creating an accurate medical summary and extracting action items. It eliminated the need for manual note-taking and provider involvement in medical documentation.
2. Natural Language Processing (NLP) Technology
The eCareScribe AI notetaker has been trained on healthcare terminologies; it leveraged NLP (Natural Language Processing) to ensure consistency and accuracy in the language used, which helped reduce documentation errors and met compliance standards.
3. Seamless EHR Integration
The eCareScribe software seamlessly integrated with the practice’s EHR and enabled automatic medical note updates to the patient profile. This centralized, real-time, and accurate medical documentation for healthcare providers to access patient medical records at any time to make informed decisions, and customize the treatment plans. This resulted in improved care delivery and ultimately increased patient satisfaction and engagement.
Value Delivered
Implementing eCarescribe AI Notetaker transformed the practice’s operations by relieving providers of their extensive documentation duties. The benefits realized included:
1. 50% Reduction in Documentation Time
By automating the note taking process, providers saved 1 hour an average per day, allowing them more time for patient care and reducing after-hours work.
2. Enhanced Provider Satisfaction
With reduced administrative demands, provider satisfaction increased significantly. Staff turnover decreased by 30%, fostering a more stable care environment and improving care continuity.
3. Improved Data Accuracy and Compliance
The AI-powered notes ensured consistent documentation quality, reducing compliance risks and improving the accuracy of patient records.
4. The AI-powered notes ensured consistent documentation quality, reducing compliance risks and improving the accuracy of patient records.
Providers could focus more on patient interactions and care quality, contributing to better patient outcomes and satisfaction.



